Ischemic heart disease, also known as coronary artery disease, is the leading cause of death worldwide. It occurs when the coronary arteries narrow due to plaque buildup, leading to reduced blood flow to the heart muscle. This condition can cause chest pain, also called angina pectoris, and increase the risk of myocardial infarction, heart failure, and sudden cardiac death.
Understanding the risk factors, symptoms, and treatment options is crucial for managing this condition effectively. This article explores ischemic heart disease in detail, covering everything from its causes to the latest surgical treatments and lifestyle changes for better heart health.
What Is Ischemic Heart Disease?
Ischemic heart disease, sometimes called coronary heart disease, develops when the coronary arteries cannot supply blood efficiently due to obstructive coronary artery disease. This condition leads to cardiac ischemia, where the heart muscle does not receive enough blood rich in oxygen. Over time, it can cause serious complications such as heart attack and heart failure. Reduced blood flow can also lead to complications such as blood clots.
Types of Ischemic Heart Disease
- Stable angina (Stable ischemic heart disease)
- Predictable chest discomfort during physical activity or emotional stress.
- Usually relieved by rest or calcium channel blockers.
- Acute coronary syndrome (ACS)
- A more severe form of ischemic heart disease, which includes:
- Unstable angina (unexpected chest pain that occurs at rest).
- Myocardial infarction (heart attack caused by a blocked artery). Narrowed arteries can lead to inadequate blood supply and ultimately result in heart attacks, which may present with classic symptoms like chest pain and shortness of breath, or minimal to no symptoms.
- Sudden cardiac death due to abnormal heart rhythms.
- Silent ischemia
- Developing silent ischemia occurs when reduced blood flow does not cause noticeable symptoms.
- Often detected through a stress test or cardiac catheterization.
Causes of Ischemic Heart Disease
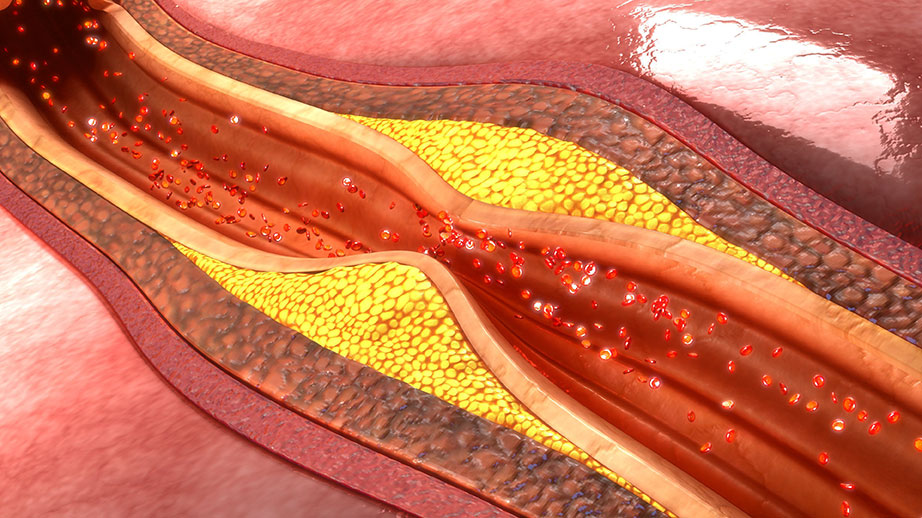
1. Atherosclerosis (Plaque Buildup)
Called atherosclerosis, this condition occurs when plaque buildup in the artery walls narrows the blood vessel, reducing blood flow. Over time, these deposits harden and make it harder for the coronary arteries to supply blood efficiently.
2. Blood Clot (Thrombosis)
A blood clot may form over a ruptured plaque, blocking blood flow completely. This can lead to myocardial infarction, a severe complication of ischemic heart disease.
3. Coronary Artery Spasm
A sudden tightening of the coronary arteries restricts oxygen-rich blood supply. This can cause angina pectoris or myocardial ischemia.
4. Endothelial Dysfunction
Damage to the blood vessel lining affects how the coronary arteries supply blood to the heart muscle.
Risk Factors for Ischemic Heart Disease
Modifiable Risk Factors
- High blood pressure damages the artery walls, increasing the risk of coronary artery disease.
- High cholesterol contributes to plaque buildup in the coronary arteries.
- Smoking harms the cardiovascular system and increases the risk of coronary blockages.
- Diabetes accelerates the progression of ischaemic heart disease.
- Obesity leads to high blood pressure, high cholesterol, and heart disease.
- Physical inactivity contributes to poor heart health and cardiovascular events.
- An unhealthy diet rich in saturated fat increases plaque buildup.
- Emotional stress triggers angina pectoris and abnormal heart rhythms.
Non-Modifiable Risk Factors
- Family history significantly increases the risk of coronary artery disease.
- Age—men over 45 and women over 55 have an increased risk.
- Gender—men are at higher risk, though postmenopausal women also face a higher likelihood of developing silent ischemia.
Symptoms of Ischemic Heart Disease
Common Symptoms
- Chest pain (angina pectoris), which may feel like pressure or tightness, especially during physical activity.
- Shortness of breath due to reduced blood flow.
- Extreme fatigue as the heart struggles to pump blood efficiently.
- Heart palpitations caused by irregular heart rhythm.
Atypical Symptoms
Some individuals, particularly women, diabetics, and older adults, may experience:
- Jaw, neck, or shoulder pain.
- Dizziness or lightheadedness.
- Indigestion or nausea.
- Cold sweats.
Silent Ischemia
Silent ischemia occurs when there are no noticeable symptoms, making stress tests and physical exams critical for diagnosis.
Diagnosis of Ischemic Heart Disease

1. Medical History and Physical Exam
Doctors assess risk factors such as family history, high blood pressure, and high cholesterol levels.
2. Electrocardiogram (ECG/EKG)
Detects abnormal heart rhythms and signs of myocardial ischemia.
3. Stress Test
Evaluates how the heart responds to physical activity, detecting silent ischemia.
4. Echocardiogram
Uses ultrasound imaging to assess the heart muscle’s function.
5. Coronary Angiography
A cardiac catheterization procedure that visualizes blocked arteries.
6. Blood Tests
- Troponin levels—indicate heart attack.
- Lipid profile—measures cholesterol levels.
- Blood sugar—assesses diabetes risk.
7. Coronary CT Angiography
Coronary CT angiography is a cutting-edge, non-invasive imaging test that provides detailed pictures of the coronary arteries. This test is instrumental in diagnosing coronary artery disease, pinpointing the exact location and severity of blockages. It also helps identify other conditions like coronary artery aneurysms or malformations.
During the procedure, a contrast agent is injected into a vein in your arm. As the agent travels through the coronary arteries, X-rays capture detailed images, which are then reconstructed into a 3D model. This allows doctors to visualize any blockages or abnormalities with precision.
The advantages of coronary CT angiography are numerous:
- Non-Invasive: Unlike traditional methods, this test does not require surgery or catheter insertion into the coronary arteries.
- Detailed Imaging: It provides high-resolution images, aiding in accurate diagnosis and treatment planning.
- Versatility: Besides detecting coronary artery disease, it can identify other coronary conditions.
- Monitoring: It is useful for tracking the progression of coronary artery disease over time.
However, it’s important to note the risks involved. The test exposes patients to radiation, which can increase cancer risk. Additionally, the contrast agent may cause allergic reactions or kidney damage in some individuals.
Complications of Ischemic Heart Disease
Ischemic heart disease can lead to several severe complications, each with its own set of challenges:
Treating Coronary Artery Disease
1. Lifestyle Changes
- Heart-healthy diet low in saturated fat.
- Regular physical activity improves blood flow.
- Smoking cessation to prevent coronary artery disease progression.
- Stress management reduces abnormal heart rhythms.
2. Medications
- Aspirin prevents blood clot formation.
- Statins lower high cholesterol and slow plaque buildup.
- Beta-blockers reduce high blood pressure.
- Calcium channel blockers help widen blood vessels.
3. Surgical Treatments
- Percutaneous coronary intervention (PCI): Also known as angioplasty, this minimally invasive procedure opens blocked arteries.
- Coronary artery bypass graft (CABG): Also known as coronary artery bypass, this bypass surgery reroutes blood flow around blocked arteries.
Prevent Coronary Artery Disease
1. Maintain a Healthy Diet
- Increase fiber intake and reduce saturated fat consumption.
2. Exercise Regularly
- Engage in at least 150 minutes of moderate physical activity per week.
3. Monitor and Control Risk Factors
- Keep blood pressure, cholesterol, and blood sugar in check.
4. Avoid Smoking and Excess Alcohol
- Smoking damages artery walls and increases the risk of coronary complications.
Emerging Treatments and Prevention Strategies
The landscape of treating coronary artery disease is evolving with several promising treatments and prevention strategies:
Conclusion
Ischemic heart disease is a serious condition that requires early detection and proactive management. By following clinical practice guidelines, making lifestyle changes, and adhering to prescribed treatments, individuals can significantly reduce their risk of serious complications such as sudden cardiac death.
Regular physical exams, stress tests, and cardiac catheterization procedures help detect obstructive coronary artery disease before it leads to a heart attack. Whether through coronary artery bypass graft surgery, percutaneous coronary intervention, or medications, treating coronary artery disease can greatly improve blood flow and overall heart health.
If you experience chest discomfort, shortness of breath, or extreme fatigue, seek medical attention immediately to prevent a life-threatening cardiovascular event.
Expert Heart Care, Personalized for You
Your heart works hard for you—let us help you keep it strong. At New York Choice Medical, we offer comprehensive heart health assessments, cutting-edge diagnostics, and customized treatment plans to prevent and manage ischemic heart disease. Don’t ignore the signs—improve your heart health today by booking a consultation with our specialists. Visit nychoicemedical.com to get started!
Frequently Asked Questions (FAQ) About Ischemic Heart Disease
2. What are the early warning signs of ischemic heart disease?
The most common early signs include:
- Chest pain or chest discomfort, especially during physical activity.
- Shortness of breath, even with minimal exertion.
- Extreme fatigue and weakness.
- Irregular heart rhythm or palpitations.
- Silent ischemia, where there are no symptoms but reduced blood flow is detected through tests like a stress test or cardiac catheterization.
3. What are the most effective ways to prevent coronary artery disease?
To prevent coronary artery disease, consider the following lifestyle changes:
- Maintain a heart-healthy diet low in saturated fat and high in fiber.
- Engage in regular physical activity, at least 150 minutes per week.
- Monitor and manage high blood pressure, high cholesterol, and diabetes.
- Avoid smoking and limit alcohol intake.
- Reduce emotional stress through relaxation techniques such as meditation or yoga.
4. How is ischemic heart disease diagnosed?
Doctors use several tests to diagnose ischemic heart disease, including:
- Medical history and physical exam to assess risk factors.
- Electrocardiogram (ECG/EKG) to detect abnormal heart rhythms.
- Stress test to evaluate how the heart functions under exertion.
- Echocardiogram to check heart muscle function.
- Coronary angiography (cardiac catheterization) to visualize blocked arteries.
5. What are the treatment options for ischemic heart disease?
Treatment depends on the severity of the disease and may include:
- Medications such as aspirin, statins, beta-blockers, and calcium channel blockers to improve blood flow and reduce the risk of coronary events.
- Lifestyle changes, including diet modification, exercise, and smoking cessation.
- Percutaneous coronary intervention (PCI) (angioplasty) to open blocked arteries.
- Coronary artery bypass graft (CABG), a surgical treatment that reroutes blood flow around blocked arteries.
If you have concerns about ischemic heart disease, consult a healthcare professional for an evaluation and personalized treatment plan.